Abstract
Background
Sickle cell disease (SCD) is a blood disorder characterized by chronic hemolysis and vaso-occlusion, causing both acute complications and chronic end organ damage. This can result in impairment of functional capacity of persons with sickle cell disease (PWSCD), rendering them incapable of performing activities of daily living (ADL). This can impact their quality of life and disease prognosis. Social challenges that may occur with SCD complications include isolation and depression, caregiver fatigue, and loss of income generating capacity/employment. ADL impairment is more prevalent in non-Hispanic Black people compared to White people. The current prevalence of ADL impairment in adults with SCD is unclear. Screening for impaired ADLs may be an efficient approach to identifying PWSCD requiring additional services to maximize their function and independence.
Objective
To determine the prevalence of ADL impairment among PWSCD receiving care at the comprehensive SCD clinic at Duke University Hospital (DUH) and evaluate associations between ADL impairment and complications of SCD.
Methodology
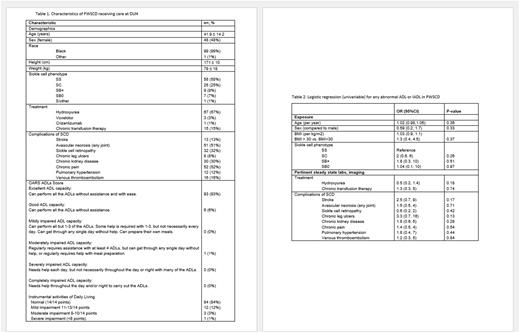
This was a retrospective cohort study. We randomly reviewed 100 electronic health records (EHR) of adult PWSCD with recorded 14-item Older Americans Resources and Services score (OARS) Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) data. Data were manually abstracted from the EHR and entered in REDCap for secure storage. Information collected included demographics, SCD genotype, steady-state laboratory and imaging results, treatment, number of hospital visits, complications of SCD as documented on the patient's problem list and/or clinician note, and OARS ADL score as reported by the patient or their surrogate. ADL impairment was defined as dependence in one or more ADL or IADL. We analyzed the data in Stata SE 17 (StataCorp, College Station, TX) using descriptive statistics and evaluated the association between Impairment in ADL and complications of SCD using logistic regression.
Results and Discussion
Data were collected from 100 records (Table 1); 52% were male (n=52). The mean age was 42 (SD 14.2 years, range 19 - 71). Most PWSCD were African American (99%). The most common variant of SCD was HbSS (58%), followed by HbSC (25%), HbSBplus (9%), and HbSBnull thalassemia (7%). Most participants were on hydroxyurea (67%), and 15% were on chronic transfusion therapy. Most patients (86%) were hospitalized 0 to 3 times/year (86%), (4-6, 10%; 7-10, 2%; >10, 2%). Twelve patients (12%) were seen in the ED seven or more times/ year, and 14% had at least seven day-hospital visits primarily for pain management. The most common health complication was chronic pain (52%), followed by avascular necrosis of the hip (57%), and 20% had a history of joint surgery. We identified basic ADL impairment in 7% and IADL impairment in 16% of PWSCD. The most common impairments were in IADLs such as traveling to places beyond walking distance (6%), going shopping (6%), preparing meals at home (7%), and doing housework (12%). PWSCD with HbSS had the most frequent hospital visits and chronic pain, and those with HbSC disease and SB+ thalassemia had the highest likelihood of having sickle cell retinopathy. No measured variables were significantly associated with ADL impairment, including demographics, baseline laboratory values, or SCD complications. In the Cardiovascular Heart Study, impairment in IADLs was slightly lower than the 24% prevalence in community-living older adults (age > 65 years, mean 74 years).
Conclusion
This study identified impairments in ADLs and IADLs in PWSCD in a comprehensive sickle cell program. Despite a mean age of 41 years, the proportion with impairment in instrumental ADLs was similar to that seen in older adults. Of note, the OARS ADL score may have missed identifying some unique aspects of ADL impairment experienced by PWSCD, like sleep deprivation due to chronic pain. Our power to detect associations was limited by the limited number of participants with impairments in ADLs, and the prevalence of ADL impairment may have been underestimated if PWSCD with ADL impairment had fewer routine clinic visits. These limitations further emphasize the need for creating a tailored functional assessment for PWSCD and future research to assess the impact of supportive and rehabilitative interventions to improve and preserve functional independence and overall quality of life.
Disclosures
Strouse:Takeda: Consultancy.
Author notes
*Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal